December 1st is World AIDS Day
By Mark Brennan-Ing, PhD, Director for Research and Evaluation, ACRIA Center on HIV and Aging
Latinos are the largest and fastest growing ethnic group in the U.S., and comprise 17% of the population. They are often viewed as a monolithic group by mainstream culture. However, the term Latino, referring to people of Mexican, Central American, and South American origins, encompasses great diversity with regard to nationality, immigration history, language use, educational and occupational opportunities, and socio-economic position. These aspects of diversity also serve as indicators of social-structural determinants of health disparities (or differences in how often a disease affects people). How these social-structural determinants of health affect the lives of older Latino adults help us to better address the needs of this population. Understanding health disparities also provides insight into challenges faced by diverse elders from a variety of racial, ethnic and cultural backgrounds who deal with many of these same issues. The intersection of HIV/AIDS and depression among older Latinos will be used to illustrate how these social-structural determinants affect the health and well-being of a diverse aging population.
Double Jeopardy: HIV and Depression
Latinos are disproportionately affected by HIV/AIDS. The overall HIV prevalence rate for Latinos is nearly three times the rate for whites. Further, Latinos are the most likely to be classified at Stage 3 (i.e., AIDS) at the time of their HIV diagnosis (48%), as compared with whites (42%) and blacks (39%). Due to successful anti-retroviral therapy, by 2015 more than half of those with HIV in the U.S. will be 50 years or older, a proportion that will rise to 70% by 2020. The disparity in HIV prevalence is amplified among older people with HIV/AIDS. Among Latinos who are 50 and older, HIV prevalence is five times that of older non-Hispanic whites. In addition, older Latinos have a 44% increased risk for major depression and are more likely to present with clinically significant depressive symptoms compared with older whites. This syndemic (convergence of two disorders that magnify the negative effects of each) of HIV and mental distress among Latino older people with HIV (“OPWH”) is an important public health concern since the most consistent predictor of HIV treatment non-adherence is depression, and only 26% of Latinos with HIV achieve the clinical goal of viral suppression.
HIV and mental health disparities among Latino OPWH arise from a common set of social-structural determinants (e.g., national origin, education, income). Disparities in both HIV prevalence and depression are associated with national origin. For example, Puerto Ricans are disproportionately affected by HIV in the U.S. relative to other Latinos, and are at greater risk for depression compared to Mexican- or Cuban-Americans. Lower socioeconomic position (SEP) is linked to higher rates of HIV infection in Latino communities, and inadequate economic resources imparts the greatest risk for depression in this population. Other social determinants of both HIV infection and depression among Latinos include immigration history and acculturation.
Research on Older Latinos with HIV
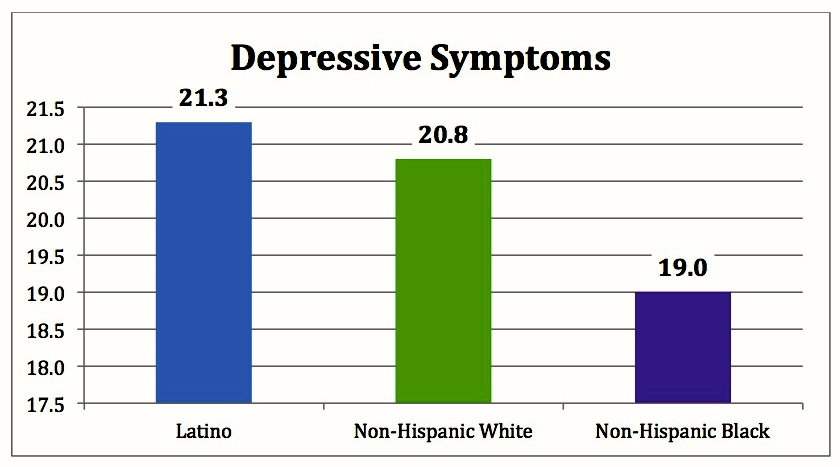
These disparities are evident in research that we have conducted at the ACRIA Center on HIV and Aging. Findings from our landmark Research on Older Adults with HIV (ROAH) study show that older Latinos with HIV were more than 3 times as likely to be foreign-born (37%) and more than five times as likely to have less than high-school educations (27%) compared with non-Hispanic whites (11% and 5%, respectively). These differences in social-structural determinants of health are evidenced by findings that older Latinos with HIV were more likely than non-Hispanic blacks to have an AIDS diagnosis (52% and 46%, respectively). In terms of immune system functioning as measured by CD4 t-cell counts, older Latinos had the lowest counts on average (313) compared to non-Hispanic blacks (492) or whites (449). In terms of mental health, older Latinos in the ROAH study reported the highest average level of depressive symptoms among the three major racial/ethnic groups. Nearly half of older Latinos (46%) met the threshold for severe depressive symptoms compared with 40% of non-Hispanic whites and 35% of non-Hispanic blacks.
In some recent work, we’ve examined the impact of social-structural factors on health disparities between older Latinos and non-Latinos in the ROAH study using economic decomposition analyses. In these analyses, we examined differences on CD4 counts and depressive symptoms. The analyses also account for the previously mentioned social-structural factors, and included age, education, employment status, and prior AIDS diagnosis. Even after accounting for these factors, disparities between Latinos and non-Latinos persist regarding immune function and mental health; a phenomenon known as “statistical discrimination.” Simply put, statistical discrimination represents an additional degree of health disparity that older HIV-positive Latinos face relative to their non-Latino peers. And it is very likely that this effect was conservatively estimated with the ROAH data, as all Latinos who participated spoke English and we did not see any significant racial/ethnic differences in current use of HIV medications indicating similar levels of access to care.
The Need for More Research
While we have been able to quantify the effects of statistical discrimination responsible for health disparities in immune function and mental health between older Latinos with HIV and their peers, we still have not been able to identify the sources of such discrimination. Yet such information is vital in order to improve treatment outcomes and quality-of-life for older Latinos with HIV. Being able to identify the sources of these disparities will also help to inform policies and programs targeting other communities of diverse elders who face similar challenges as older Latinos due to culture, language, and immigration history. Armed with such information, we will be in a better position to support older adults of all backgrounds to successfully face the challenges of aging.
Mark Brennan-Ing, PhD is the Director for Research and Evaluation at the ACRIA Center on HIV and Aging. The opinions expressed in this article are those of the author and do not necessarily reflect those of the Diverse Elders Coalition.